Bronchiolitis

Bronchiolitis is a very common illness in babies.It is caused by a virus. The most common one is called respiratory syncytial virus (RSV) but lots of other "common cold" viruses can also cause the illness.The virus infects the small airways of the lungs (called "bronchioles") causing them to become inflamed, blocked with mucus and narrowed. Due to this, babies must work harder to breathe which can be seen as a fast breathing rate, sucking in of the ribs and noisy breathing. Over time, they can become tired, develop low oxygen levels, have reduced feeding and become dehydrated.Worldwide, bronchiolitis is the most common reason for babies to need admission to the intensive care unit (ICU). Paediatric and intensive care doctors are very used to looking after babies with this condition.
Treatments

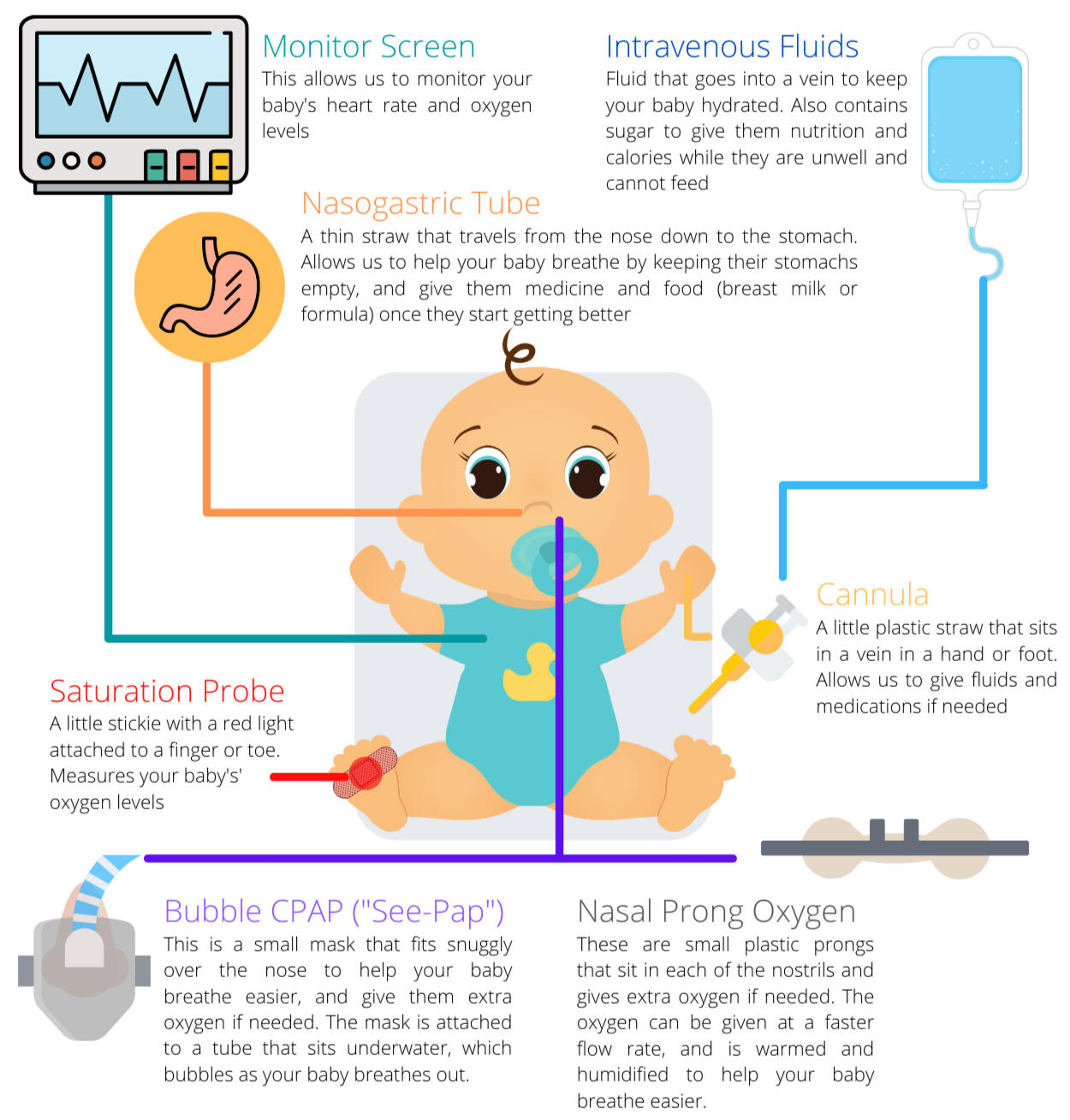
Help with breathing
Some babies need help with their breathing or may need extra oxygen. This can be provided by using breathing devices which are placed on the nose or face, called bubble CPAP or nasal prong oxygen (see section on equipment below).
Nose suction
Young babies and infants have not learnt to breathe through their mouth yet, so it is important to keep their nose clear of secretions. Nurses might use saline drops (salty water) put into the nostrils to help loosen the secretions, and perform gentle suctioning using a soft plastic straw called a catheter.
Medicine to treat fever and discomfort
Fever itself does not cause harm to babies and is part of their body's way of fighting infection. However having a fever can make some babies feel miserable and make their breathing become faster and more laboured. If this occurs, a medication such as paracetamol (acetominophen) or ibuprofen may be given to help make your baby feel more comfortable.
Food
Babies in ICU get hungry and feeding them is always preferred. However in some babies who are working hard, a full stomach pushes upwards on the lungs and diaphragm and makes breathing worse. In this case, feeding might be temporarily withheld. Medical staff will keep a close eye on your baby's hydration and give intravenous fluids. Once breathing starts to get better, feeding is slowly reintroduced by using either expressed breast milk (EBM) or formula which is given down the nasogastric tube into the stomach (see section on equipment below). The volume of feeds are kept small at first and are slowly increased over time.
Sedation
Being upset and crying makes breathing worse. Therefore, infants are sometimes given a mild sedating medicine to help them feel more comfortable and settled. The medicine does not have any long-term side effects.
Inhalers
Asthma inhalers don't work in bronchiolitis. However in older children, the symptoms of bronchiolitis can overlap with a seperate but similar breathing condition called viral-induced wheeze (VIW). In this setting, doctors might try an asthma inhaler to see if it helps the airways open up. Please note that the presence of wheeze or a response to inhalers does not mean that your child has asthma nor that they will have asthma in the future.
Antibiotics
Because bronchiolitis is caused by a viral infection, antibiotics do not help. However, some babies can develop a second bacterial infection on top of the bronchiolitis and may require a short course of antibiotics. This might be given intravenously or into the stomach through the nasogastric tube (see section on equipment below).

Meet the team
Nurses
A highly trained ICU nurse stays at your baby's bedside all day and night. They look after all aspects of your baby's care including managing breathing, giving medicines, fluids, and feeding.
Doctors
ICU doctors and paediatric doctors work closely together to provide care to your baby. You will usually see them on "ward rounds" where they come to see your baby (usually in big groups) and make treatment plans for the day.
Other team members
Many other important people work behind the scenes to ensure your baby receives the care they need. These include physiotherapists, cleaners, health-care assistants, pharmacists, dieticians, medical and nursing students and phlebotomists. You will no doubt meet some of them.
Tests
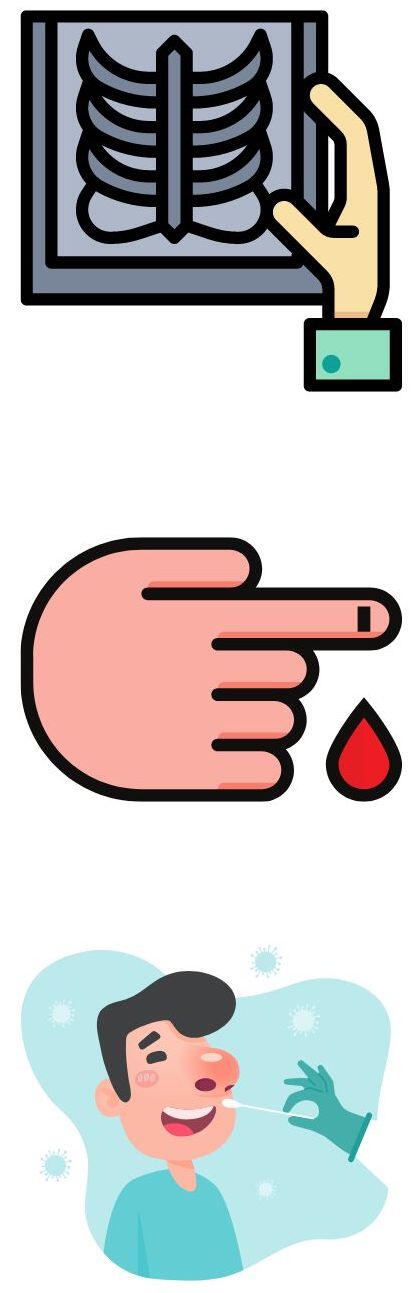
X-rays
Chest X-rays are not routinely performed, however one might be done so that doctors can check to see if there are signs of a second bacterial infection or other lung issues. The amount of radiation used for a baby chest X-ray is very small.
Blood test
Blood tests may be needed to check your baby's blood sugar levels, electrolyte levels and kidney function. This usually involves a small prick of the heel done by either nurses or phlebotomist (clinicians who specialist at doing blood tests).
Nose Swab
A nose swab is usually taken to rule out COVID and to test for some of the common viruses, however it is not possible to test for all the viruses that cause bronchiolitis because there are so many types. The result of the nose swab does not change treatment but will help the ICU team make decisions about whether your baby needs isolation to protect other children from also getting the illness.
Expected Course

Bronchiolitis typically peaks in severity on day 3 of the illness so some babies can get worse before they get better. Most babies will spend around 3 to 5 days in ICU before they have improved enough to be discharged to the children's ward.A very small number of babies might get sicker and develop critically low oxygen levels or breathing fatigue. These babies may require a breathing tube and need to be put onto a breathing machine (called a ventilator) to help them.It is useful to note that bronchiolitis is extremely common and the vast majority of children will have a straight forward course and make a complete recovery with no lasting effects. Your nurse and doctor will be able to give you updates regularly and let you know how things are going.
Common Questions

Is bronchiolitis contagious?
Yes, the viruses that cause bronchiolitis are spread through respiratory secretions and therefore babies are contagious while they have symptoms such as a runny nose or cough. Other children are at the most risk of catching the illness. Because most adults have had these viruses before, they may be immune and might not get sick. It is important to prevent spread of the virus with good hand washing or by using hand gel when you enter or leave your baby's bed space.
Can my baby get it again?
Some babies only have bronchiolitis once in their life, however others may have many episodes as they come into contact with different cold viruses as they grow up. Usually each new episode of bronchiolitis becomes less severe as children get older and their airways and lungs get larger.
Can I breast feed my baby?
Breast feeding is always promoted, however some babies are too unwell to do so because they are working hard to breathe. Mums are encouraged to express breast milk so that it can be stored and given to baby later once they are ready to start feeding. Infant formula is available for babies that are not breast fed.

Author
Dr Pras Mao
Pras is a specialist consultant in paediatric intensive care, paediatric emergency medicine, adult intensive care and adult emergency medicine. He has completed fellowships at Starship Children's Hospital, Middlemore and Wellington ICU. He likes to design clinical tools using human-factors based concepts to make work and life simpler.